Cataracts
This guide will help you learn more about:
- how cataracts develop
- how cataracts are treated with surgery
- what kind of costs to expect, and
- how long it will take you to recover from surgery
The information will help you be more educated and involved in your eye doctor’s treatment through diagnosis, surgery and recovery.


What is a Cataract?
A cataract is a clouding of the eye’s lens, which blocks or changes the passage of light into the eye. The lens of the eye is located behind the pupil and the colored iris, and is normally transparent. The lens helps to focus images onto the retina – which transmits the images to the brain.
Your vision may become blurry or dim because the cataract stops light from properly passing through to your retina.
How common are cataracts?
Cataracts are a leading cause of blindness among older adults in the United States. More than half of all Americans have cataracts by the time they are 80 years old. Cataracts can also sometimes be found in young people or even newborn babies.
Am I at risk for developing cataracts?
The exact cause of a cataract is unknown. Most often, a cataract is part of getting older. As you age, you are at greater risk of developing a cataract. There are also several possible risk factors for cataracts, such as:
- Intense heat or long-term exposure to UV rays from the sun
- Certain diseases, such as diabetes
- Inflammation in the eye
- Hereditary influences
- Events before birth, such as German measles in the mother
- Long-term steroid use
- Eye injuries
- Eye diseases
- Smoking
What are the symptoms of a cataract?
Generally, a cataract does not cause pain, redness or tears. The following problems may indicate that you have a cataract:
- You have blurred vision, double vision, ghost images, or the sense of a “film” over your eyes.
- Lights seem too dim for reading or close-up work, or you are “dazzled” by strong light.
- You change eyeglass prescriptions often and the change does not seem to help your vision.
- You may also be able to see the cataract in your eye. It may look like a milky or yellowish spot in your pupil.
Why do cataracts form?
Cataracts are probably caused by changes related to aging. Throughout our lives, our bodies replace old cells with new ones. As we grow older, the old cells in our eye’s lens build up and block light as it tries to pass through. The end result is cloudy vision.
Besides getting older, other factors may cause cataracts to form. Eye infections, some medicines (such as steroids), injuries or exposure to intense heat or radiation may cause cataracts. Too much exposure to non-visible sunlight (called UV or ultraviolet light) and various diseases, such as diabetes or metabolic disorders, may also contribute to cataracts forming.
What are the types of cataracts?
Age-related – 95% of cataracts are age-related, usually after age 40.
Congenital – These are present at birth, usually caused by infection or inflammation during pregnancy; possibly inherited.
Traumatic – Lens damage from a hard blow, cut, puncture, intense heat or chemical burn may cause cataracts.
Secondary – Some medicines, eye disease, eye infection, or diseases such as diabetes cause these cataracts.
Cataracts usually form in both eyes, but not at the same rate. They can develop slowly or quickly, or progress to a certain point, then not get any worse. As a result, you may not notice large changes in your sight right away.
How will my eye doctor check for cataracts?
Everyone who gets a cataract experiences it differently. But a person with a cataract commonly experiences cloudy or blurry vision. Lights may cause a glare, seem too dim or seem too bright. It may be hard to read or drive, especially at night. If you have a cataract, you may see halos around lights, such as car headlights, that make it hard to focus clearly. Colors may not seem as bright as they used to be. Or you may have to change your eyeglass prescription often.
If you notice any of these changes, make an appointment to see your eye doctor.
If you have a cataract, you may have symptoms that are similar to those of other eye diseases. Only your eye doctor can tell you for sure what’s wrong.
To find out if you have cataracts, your eye doctor will want to:
- find out your general medical history
- find out your specific eye history, including problems and symptoms
- test your vision (visual acuity)
- test your side vision (peripheral vision)
- test your eye movement
- test you for glaucoma (by measuring the eye’s internal pressure)
- do a microscopic exam of the front of the eye (using something called a slit lamp) to assess the density of the cataract and how it interferes with light passing through the lens
- widen (dilate) the pupils of your eyes to examine the retina, the optic nerve (which carries visual messages from the retina to the brain) and the macula (responsible for the best part of central vision)
- test you to see how glare affects your vision
After this exam, your eye doctor will determine whether you have cataracts, how much they interfere with your vision, whether surgery would help, and what types of treatment and lens replacements are best for you.
Cataracts and Vision Loss
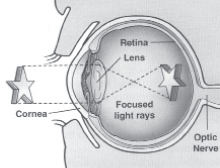
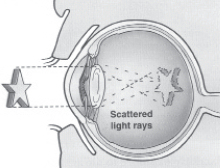
Your eye works like a camera. A camera needs a lens to focus an image. But when the lens is dirty or cloudy, the camera can’t take a good, clear picture.
It’s the same with your eyes. Your eye lens focuses rays of light on the nerve tissue at the back of your eye (the retina). The retina then transmits a clear image to your brain. But when a cataract clouds your eye’s lens, light rays don’t pass through as well and the retina cannot transmit a good picture.
About one in six Americans age 40 and older will get a cataract. By age 80, more than half will have a cataract. Because everyone is different, some people may not notice a large change in their eyesight. Others will find it a challenge to enjoy even the simplest tasks and may find it harder and harder to stay independent.
Light passes through a normal eye
without anything blocking its way.
When the lens of your eye becomes cloudy,
the cataract prevents you from seeing clearly
by preventing enough light from passing through.
Cataract Surgery
Cataract surgery has restored vision to millions of people. Every year in the U.S., more than two million cataract surgeries are performed.
The key to preventing vision loss is regular eye exams. If you are 65 or older, you should get a complete eye exam every one or two years, even if you have no problem seeing well. Be sure to ask your eye doctor for a dilated eye exam.
Every year in the U.S., more than two million cataract surgeries are performed. Cataract surgeries are performed without complication in over 95% of cases. Still, you will likely have questions, fears or reservations about the procedure.
Should I Have Cataract Surgery?
It is your choice to have cataract surgery.
Cataracts will not cause large vision changes for some people. A cataract at the outer edge of your lens, for example, may hardly affect your vision. A cataract at the center of your lens, may greatly affect your sight.
You should only agree to have surgery when you are unable to do all the things you want to do while wearing your glasses. If you decide to have surgery, you and your eye doctor (for cataract surgery, this will be an ophthalmologist or eye MD), must work together as a team.
An ophthalmologist is a medical doctor who specializes in diseases of the eye. He or she has been trained as an eye surgeon to perform cataract surgery.
You and your eye doctor will determine the best treatment for you—the one you are most comfortable with and the one he or she is best at performing. As you read this guide, note any questions or concerns you may have and discuss them with your eye doctor.
Note: If a cataract keeps an eye doctor from viewing the inside of your eye, he or she may suggest surgery.
Your eye doctor needs to be able to view the inside of your eye to check for eye diseases such as glaucoma and problems of the retina (the innermost part of the eye containing lightsensitive nerve cells).
When Can I Avoid Cataract Surgery?
Prevent Blindness America recommends that individuals do not have cataract surgery if:
- cataracts have not affected your lifestyle or kept you from doing all the things you want and need to do
- your vision will not improve with surgery because of other eye problems
- glasses or contact lenses can provide satisfactory vision
- you are not well enough/fit enough for the surgery
- you do not want surgery
Cost of Surgery
Basic charges you can expect for cataract surgery include fees for the hospital/surgical center, the doctor, the anesthesiologist, basic tests before surgery, medicine after surgery and followup visits with your doctor. Ask your doctor to estimate each of the costs. You may also need new glasses or contact lenses after surgery.
If you have private health insurance or Medicare, it will usually pay for a part of most costs. Try to find out what your health insurance will cover before the surgery. Extra insurance (secondary supplemental insurance) also may cover 80% of the amounts not covered by your primary insurance. You may have to pay 20% of the balance. Ask your doctor about his or her billing and payment methods. Newer “bifocal” IOLs are not usually covered by insurance.
Some hospitals and surgical centers may be able to help you with financial planning. This may include putting together a payment plan or filing claims to your insurance company. Filling out insurance forms can be hard—so be sure to ask questions ahead of time.
Follow-up Care
Your doctor will suggest a schedule for follow-up visits. The first one will be the day after your surgery. It is important to keep these appointments to find out whether your eye is healing well. These visits will also let you ask your doctor any questions you have about medicine or your activities (such as heavy lifting or exercising).
Enjoy Better Vision
Your vision will be blurry right after your operation. But each day it will get sharper and clearer. How well you see right after surgery does not necessarily relate to how well you will see later on. But better vision soon after your operation is a good sign.
As your eye heals, you may find yourself seeing better than you have in a while. Everything may seem brighter and clearer. It’s likely that your sight will be almost as good as it was before the cataract developed, but you may still need glasses or contacts for close-up work or distance vision.
After one successful operation, many patients who need a second surgery are less nervous about it and look forward to the day they can view the world clearly, without cataracts.
Don’t be rushed into choosing surgery unless there is a medical emergency that warrants it. You should feel comfortable with your decision. That includes feeling comfortable with your doctor.
Types of Lenses
When the eye surgeon removes your cataract lens, you will need something to replace it so that you can focus and see clearly. You have three choices to replace your own lens:
Intraocular Lenses
Intraocular lenses (IOLs) replace your cataract, or cloudy lens. If you have certain eye diseases or problems which prevent safe placement of an IOL, you will need either contact lenses or cataract glasses in order to see clearly after surgery.
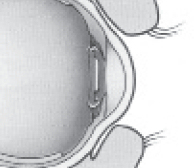
IOLs are the most popular choice for replacing lenses with cataracts. Unlike contact lenses, these lenses are implanted inside the eye and are meant to be permanent. They do not require replacement or cleaning.
The eye surgeon implants the IOL in about the same place as your natural lens, so that it results in the most natural vision.
IOLs are placed inside the eye.
IOLs are the best option to replace your own lenses. However if you have certain other eye diseases or problems, you may not be able to have lens implants. You and your eye doctor will need to discuss whether any restrictions apply.
In order to put in an IOL that exactly fits your eye, your eye doctor will measure the length of your eye before your surgery using a painless sound wave (ultrasound) test to determine what strength you will need for your IOL. Your eye surgeon will also check the health of your retina and cornea and give you an estimate of the level of vision you can expect after surgery.
The IOL may correct nearsightedness or farsightedness so that you may see well without glasses for distance vision. However, after standard IOL implantation, you will still need glasses to read clearly. Currently, there are special “multifocal” IOLs that enable you to see well not only for distance vision but also possibly for reading vision. You and your doctor will need to discuss whether this is an option for you.
Contact Lenses
If you are unable to have an IOL implant, you may opt to wear contact lenses after cataract surgery.
By wearing a contact lens on your operated eye, you will be able to see about as well as you did before the cataract developed. These lenses cannot cure all your vision problems. You may still need glasses for close-up work.
There are two types of contact lenses: daily-wear and extended-wear. You must remove daily-wear contact lenses before you go to sleep. You can wear extended-wear contact lenses for longer periods of time. Extended-wear contact lenses are usually prescribed for people who would have trouble inserting and removing daily wear contacts (for example, people with severe arthritis).
If you need to wear contact lenses after surgery, your doctor will show you how to insert and remove them, as well as clean and care for them. Learning to use contacts takes some effort. Not everyone can wear them. Contact lenses are safe and easy to use, but they can cause problems. If you have excessive redness, watering, light sensitivity or pain, you should call your eye doctor right away.
Cataract Glasses
Cataract glasses may be an option if you cannot have an IOL implant or if you cannot wear contact lenses. Cataract glasses are also safe and relatively inexpensive, but they may take some getting used to after surgery. The lenses in cataract glasses are different from regular eyeglasses, so you will see things in a different way. Objects will look larger (by about 25%) and may seem to appear suddenly in your side vision (peripheral field of vision). Vertical lines may appear curved, and it may be hard to judge distances.
If you have cataracts in both eyes but only have surgery in one eye, your eyes won’t be able to work together when you wear cataract glasses after surgery. The glasses lens for your operated eye makes things appear larger while your other eye will view images as they truly are. Your brain won’t be able to put the two images together for normal (binocular) vision. You will have this condition, called monocular aphakia (one eye without a lens), until after your second cataract operation.
Choosing a Surgeon
Once you decide to have cataract surgery, you’ll need to choose an eye surgeon to perform the operation. Some things to keep in mind are the surgeon’s experience and skill, how easy it is to talk to him or her and have your questions answered, and your previous experience with this eye doctor, if any.
Referrals may help you choose an eye surgeon. Ask friends who have had cataract surgery or contact a university with a medical school or a hospital for names and references.
If an eye doctor has recommended surgery, you may want to get a second opinion. Make an appointment to see an eye doctor who does not work with, and was not referred by, your regular doctor. You do not have to tell this doctor that someone else has already recommended surgery—let this doctor come to his or her own conclusions about whether you need cataract surgery.
Questions for Your Doctor
Here are some points you may want to bring up with your doctor. Check the questions you’d like your eye doctor to answer during your next appointment or conversation.
- Do I really need surgery? What will I gain by having it?
- What are the risks?
- What is surgery like? Will it hurt? What will I see?
- Will any other problems like glaucoma or diabetes affect my cataracts or my surgery?
- How long will I need to recover from the surgery?
- Will I need glasses after surgery? If I wear contacts, can I wear them again after surgery?
- Are there some things I won’t be able to do after surgery? If so, for how long?
- Will someone have to take care of me after surgery? If so, for how long?
- Will the medicines I take for other illnesses interfere with surgery or my recovery?
- How experienced is the doctor? Is he or she board certified?
- Is a payment plan available?
Write down any other questions you may have.
About the Surgery
Removing the cataract and inserting an intraocular lens usually takes the surgeon ten to fifteen minutes. The entire process, from arriving at the hospital or surgical center to going home, takes about half a day. Less than 1% of surgeries require an overnight hospital stay.
Before Surgery
On the day of your surgery, or a few days ahead of time, you may need to see your primary care doctor for a few tests. Because you will be given some form of anesthesia, your doctor will probably ask you not to eat or drink anything after midnight the day before your surgery. If you take medicines or have diabetes, ask your doctor whether different guidelines apply.
On the Day of Your Surgery
On the day of your surgery, you will be given some eye drops to widen (dilate) your pupils. You may also be given a mild sedative to help you relax. A healthcare worker will take you into the operating room where an anesthesiologist or nurse anesthetist will give you a local or an intravenous anesthetic. He or she will monitor your condition.
You will not feel the surgery because the topical anesthetic numbs your eye during the operation. You may see some lights or vague shapes, but that is all.
Your surgeon will use a special microscope, which magnifies and illuminates the area of the procedure as he or she removes your cataract.
After Surgery
You may not remember much about the operation after it is over. You may feel a little drowsy afterward, but as the sedative wears off, you will be encouraged to walk around a bit. Your doctor will monitor your condition for a while, explain how to care for your eye at home and schedule a follow-up appointment.
Once you’re fully recovered, you will be allowed to go home. It is a good idea to have a friend or relative drive you. You may feel tired after surgery, so try to relax the rest of the day.
At home, you should not experience much discomfort. Some people describe the feeling as having an eyelash or a cinder in their eye—slightly uncomfortable but not painful. You will apply eye drops or ointment as your doctor prescribes, and you will learn to rely on your untreated eye during this time.
Types of Cataract Removal
During the cataract operation, your surgeon will first remove the clouded lens. (If you are able to have a lens implant, your doctor will perform this procedure right after removing your cataract lens.) There are three methods for removing the clouded lens:
Phacoemulsification
The most common procedure, phacoemulsification requires a smaller incision in the cornea or, less commonly, the sclera. The surgeon uses sound waves (an ultrasonic device) to break the lens into small pieces, and then suctions the tiny pieces out through the same incision.
phacoemulsification procedure
Next, the doctor will insert the lens into place. Again, the capsular bag will remain to strengthen the eye and to preserve normal architecture. Most IOLs are foldable, so they can be inserted through the same small incision. The lens usually unfolds slowly once it is placed into the capsular bag. The incision can be closed with either one stitch, or usually none at all.
Phacoemulsification, with its smaller incision, offers the fastest healing and recovery time, produces little discomfort, and reduces the chance of uneven focus (astigmatism) or distorted vision.
Extracapsular and Intracapsular
These procedures are not often used. An extracapsular cataract extraction may be needed if your lens is too hard to phacoemalsify. The extracapsular procedure removes only the inside of the lens but leaves the capsular bag that holds the lens in place. Leaving the capsular bag adds to the structural strength of the eye and promotes easier healing. During the intracapsular procedure, your eye surgeon removes the lens and the entire capsular bag that holds it. Your doctor will make an incision in the sclera, use a special tool to freeze the lens, and then remove it through the incision. He or she may then implant the IOL in front of the iris where its loops hold it in place. Another option is to suture the IOL to the wall of the eye. This latter option enables the IOL to be placed behind the iris.
Possible Complications from Cataract Surgery
Less than 5% of patients experience complications from cataract surgery, but you should discuss possible problems with your doctor. Here are three areas of complications:
Problems During Surgery
Problems during surgery, called operative complications, such as severe bleeding, happen to less than 1% of patients. Up to 2% of patients lose the gel-like substance that fills the inside of the eye (vitreous humor) during surgery. Complication rates may be higher if you have certain medical or ocular diseases.
Problems Soon After Surgery
Problems soon after surgery, called early post-operative complications, can include leaking from the wound, bleeding or infections.
Problems After Healing
Problems after healing, called late post-operative complications, include retinal detachment (this requires surgery to correct but happens in about one out of every 100 patients), swelling of the cornea, or swelling of the retina (called cystoid macular edema). Infection is a rare complication. This happens in fewer than one in every 1,000 patients, but it may cause severe vision loss.
Sometimes after the extracapsular or phacoemulsification procedure, the capsular bag that remains in your eye can become cloudy. This is called an after cataract or posterior capsular opacification. If this happens, your doctor may suggest laser surgery to make a tiny hole through the cloudy lens capsule. This hole will let you see clearly again.
Remember, the risk of severe problems or blindness from cataract surgery is very low. Still, it may ease your mind to talk about your concerns with your doctor before surgery.
Recovery from Eye Surgery
After surgery, most of the healing takes place in the first few days. But it may take up to 1 month for your eye to fully heal. For the first week or two, or as your doctor recommends, you should minimize vigorous physical activity. You should restrict any lifting or deep bending, which causes increased eye pressure.
If you experience severe pain, loss of vision or a sudden increase in redness or swelling of your operated eye, call your eye doctor right away.
DOs and DON’Ts
- Do use your medication as directed.
- Do sit down and lift your feet to put on your shoes.
- Do try to sleep on your back or on the unoperated side.
- Do have someone else drive while your eye is healing.
- Do wear sunglasses in bright light.
- Do keep follow-up appointments with your doctor.
- Do keep moderately active.
- Don’t rub or press your eye.
- Don’t bend over to pick things up; kneel instead.
- Don’t get soap, shampoo or other irritants in your eye.
Take care of your eye
These pointers can help you recover more quickly:
Applying eye medications
Use the eye drops or ointment that your doctor prescribed to help your eye heal. This medicine protects against infection and helps decrease swelling.
How to apply eye drops or ointment
Tilt your head back. Pull your lower eyelid down to create a “cup” that holds the drops or ointment. Put in the prescribed amount of medicine and close your eye to distribute it evenly. If you have trouble doing this, ask a friend or relative for help. Start with a fresh bottle of medicine after surgery so germs don’t get transferred.
Eye shields
Your doctor may want you to use an eye shield at night to protect your eye while you sleep.